Where are We with Man Made Sperm?
“Think left and think right and think low and think high. Oh, the thinks you can think up if only you try!” Dr. Seuss
I’ve been asked to report to the fertility community about where we are with man-made sperm. Although we’re not where we’d like to be, it is certainly not for lack of trying. Around the globe, many research teams are on the quest for this Holy Grail: making sperm from scratch. There’s been some good hard science laid down that I am sure will reap rewards in the future.
How Far We’ve Come
It’s been 7 years since the first reports were published showing that normal, healthy, viable sperm can be made from stem cells in mice. In fact, pretty much any type of stem cell, adult, embryonic or otherwise, can be directed to sperm in the mouse model. And this can be done either within or even outside the testicle. Truly impressive science that is now an unrefutable accomplishment: It’s possible to make sperm from stem cells in mammals like us.
How We’re Different
But we humans, for some reason, are different. And that has made all of the difference in the progress of this science. Two general approaches have been taken to create human sperm from scratch using stem cells as seeds: putting them back into their native environment, an actual testicle of some kind (in vivo), or trying to encourage them down the path of spermatogenesis outside the body, in an recreated, artificial environment (ex vivo). Both have merit and are worth pursuing, but neither has succeeded completely (and believably) in creating a healthy, usable, mature human sperm.
Inside a Testicle
We have had partial success taking skin biopsies from azoospermic (sterile) infertile men with genetic causes and turned these skin cells into adult stem cells in a dish. From there we placed them into mice testicles (in vivo) to see if they might develop further and they have, but not very far. We then took men with genetic infertility, again turning their skin cells into stem cells, and then replaced the missing Y chromosome gene in the stem cells. Yup, actual gene therapy on stem cells. These “fixed” cells were replanted into mouse testicles and we watched them go even further along the precursor path to sperm. We never got sperm but that might simply be because mice are just too different from us for complete success. Regardless, the proof of concept is important here: these little can-do stem cells really want to progress to sperm in the right environment. Like a lawnmower ever so close to firing up when you pull the starter cord.
The University of Pittsburg is doing exciting work that uses the human testis as an incubator (in vivo). They have taken testicular stem cells from boys’ testicles before sterilizing cancer treatment and frozen them. They now plan to reimplant these cells back into the same boys’ testicles after they are cured of their cancers, hoping to grow mature sperm in the same testis that was previously sterilized. This should work, as they previously demonstrated the success of this technique in macaque monkeys. And, it starts with sperm precursor cells that are more committed to becoming sperm than say skin cells or embryonic stem cells which need extra coaxing to become sperm.
Outside a Testicle
There are published claims of mature human sperm being made outside of the testis in a dish (ex vivo) from stem cells. One study was published and then retracted in 2009 and the other sought to restart sperm production in testis tissue that was hormonally “turned off” earlier. Restarting the sperm machinery after it was turned off is not as scientifically challenging as starting from scratch and creating sperm from stem cells. It’s more like baking from a box mix but is important nevertheless.
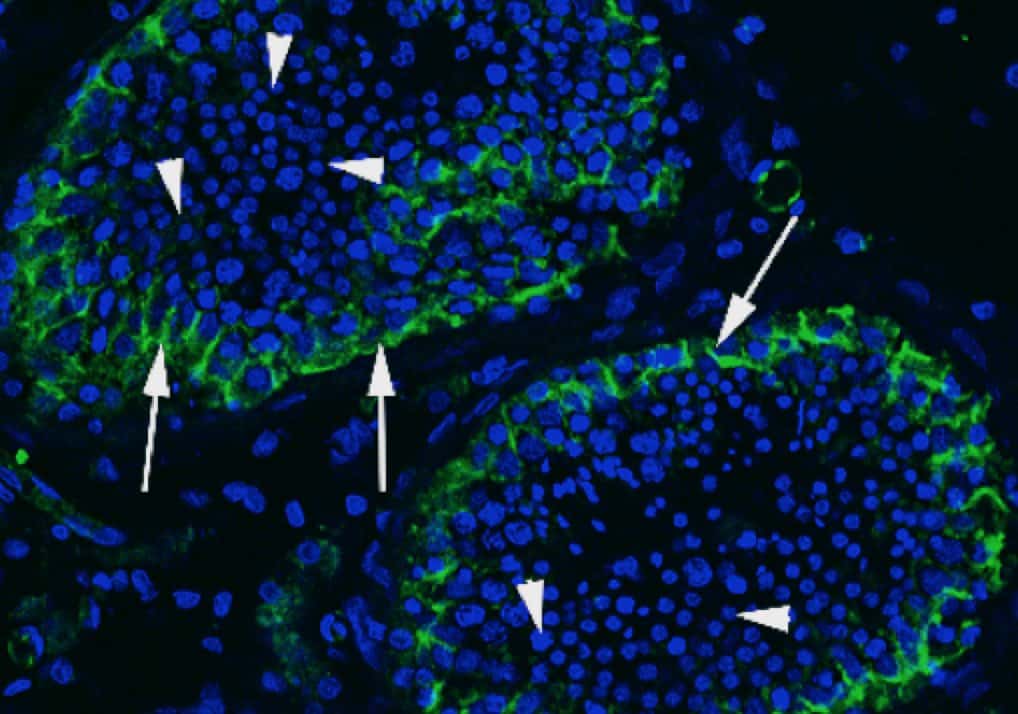
Finally, we and others, using bioreactors and organoids, have attempted to recreate the testis environment outside the human body with some success. We are now able to get all of the cells needed to make a bionic testicle and have kept it all alive for 6 weeks. And it thrived. Stems cells placed in the bioreactor not only survived but appeared to recognize the testicle-like environment in which they found themselves. But we haven’t gotten them to take the first step and take that walk toward sperm. The human testicle is an organ of mythical complexity and we will need to understand and duplicate the myriad of cell-cell interactions to make sperm.
Honestly, it’s not impossible to make man-made human sperm, it’s just more difficult than we imagined. So easy in mice, so hard in man. It’s a difference that has earned some serious scientific respect in our field. As Walt Disney said: “I only hope that we never lose sight of one thing — that it all started with a mouse.”









