Male Ejaculatory Disorders in Los Angeles & San Francisco, CA
Talk to an Expert about Ejaculatory Disorders

Having trouble ejaculating can be emotionally distressing for both you and your partner. But with the help of a qualified men’s sexual health expert like Dr. Paul Turek, relief from this issue is possible.
Types of Ejaculatory Disorders & Dysfunction
The first step toward overcoming an ejaculatory disorder is to see Dr. Turek to determine exactly what is happening and why. There may be reversible factors that are easily addressable to help you reclaim a satisfying sex life. If not, there may be medical and surgical solutions available as well. The types of ejaculatory disorders and dysfunction we treat at The Turek Clinic include:
Retrograde Ejaculation
Retrograde ejaculation is when the ejaculate or semen courses backward into the bladder instead of forward through and out of the urethra. Ideally, the bladder neck (the point where the bladder meets the urethra) should close at the moment of orgasm. However, if the nerves or muscles at the neck of the bladder are damaged, the bladder neck may not close correctly and the ejaculate ends up being sent backward into the bladder. This is not a dangerous situation but it can be upsetting as orgasm is “dry.”
Causes
- Medical conditions (e.g., diabetes, multiple sclerosis, spinal cord injury)
- Psychiatric medications, blood pressure pills or other medications
- Surgery on the prostate gland, bladder or lower abdomen
Diagnosis
A physical examination and medical history are required. Dr. Turek often orders a post-ejaculate urine sample. If sperm are present in the urine voided after ejaculation, this indicates retrograde ejaculation.
Treatment
- Oral therapy to help close the bladder neck and prevent semen from entering the bladder during ejaculation
- Discontinuing medications causing retrograde ejaculation
For couples that wish to conceive, Dr. Turek can explore the possibility of harvesting sperm from the bladder to use for assisted reproductive treatments (ART). He is also developing a simple injection technique that can restore the bladder neck anatomy to regain forward ejaculation.
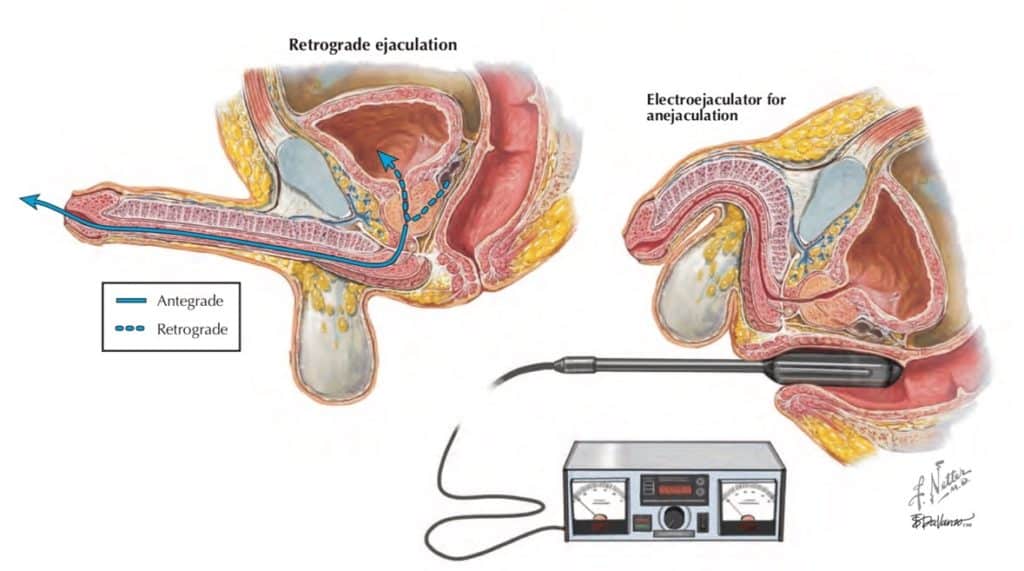
Anejaculation
Anejaculation is the absence of ejaculation and orgasm. Erections are usually normal but ejaculation does not occur despite a man’s best efforts.
Causes
- Spinal cord injury
- Certain medications (e.g., antidepressants, antipsychotics)
- Previous surgery on the prostate or bladder
- Diseases that affect the nervous system
- Psychological factors
Diagnosis
The diagnosis of anejaculation is made based on a complete medical history and physical examination. It can either be of the primary type (lifelong) or secondary (recently occurring) in nature.
Treatment
- Stopping medications that induce the condition
- Sex education and sex therapy with a counselor
- Penile vibratory stimulation or rectal probe electroejaculation to get sperm for IUI or IVF
- Surgical sperm retrieval to get sperm to use with IVF
Premature Ejaculation
Premature ejaculation is ejaculating earlier than the man would like. Usually, it is regarded as ejaculating within a minute or two after penetration. It is the most common sexual health condition in U.S. men, occurring in about one out of every three men.
Causes
- Psychological stressors like anxiety or depression
- Hormonal or metabolic conditions
- Medications or drugs
- Erectile dysfunction
Diagnosis
A detailed patient history and physical examination helps to determine whether the condition is primary (lifelong) or secondary (acquired). The evaluation includes an assessment of lifestyle and sexual habits, medical issues and medications
Treatment
- Oral medications like antidepressants (SSRIs)
- Erection medications (sildenafil, tadalafil, vardenafil) for secondary cases
- Topical (skin)_anesthetics
- Sex education with an experienced sex counselor to learn relaxation techniques and skills to control and prolong sexual stimulation. This treatment is usually curative.
Delayed Ejaculation
Delayed ejaculation is a condition in which a man takes longer than he would like to ejaculate during sexual activity. Some men may ejaculate only infrequently or not at all.
Causes
- Certain medical conditions (e.g., spinal cord injury, multiple sclerosis, nerve damage)
- Hormonal disorders (e.g., hyperprolactinemia, low testosterone)
- Medications (e.g., antidepressants, antipsychotics, alcohol)
- Back or spinal injury or surgery
- Mental health conditions like depression or anxiety

Diagnosis
Diagnosing delayed ejaculation requires a physical exam and thorough medical history. Further testing for specific underlying medical conditions may be recommended by Dr. Turek if his suspicion is high.
Treatment
- Reducing, stopping or switching from medications that affect sexual function
- Counseling with a sex therapist or educator to explore psychological issues affecting the ability to ejaculate
- Sexual retraining in alternative masturbation techniques that are more compatible with sexual stimulation
Hematospermia
Hematospermia is the finding of blood in the ejaculate. Although alarming when it occurs, it is usually painless and self-limited. The ejaculate may be bright red, brown or chocolate in color and blood clots may or may not be present.
Causes
- Urinary tract infection or inflammation of the urethra, prostate or seminal vesicles (e.g., prostatitis)
- Sexually transmitted diseases
- Anatomical issues such as urethral stricture or ejaculatory duct obstruction
- Due to testicle, urethral or prostate surgery or injury
- Prostate cancer (rarely)
Diagnosis
Dr. Turek will perform a physical exam of the genitalia and take a full medical history. Diagnostic tests may include urine and semen testing, STD tests and prostate-specific antigen (PSA) blood test and transrectal ultrasound.
Treatment
- Antibiotic therapy
- Anti-inflammatory drugs
- Reassurance
Contact The Turek Clinic
If you are having trouble ejaculating, you need the help of a dedicated men’s sexual health expert. Dr. Turek invites you to schedule a consultation at The Turek Clinic by sending us an email today.









