Genetics of Male Infertility in Los Angeles & San Francisco, CA
Male fertility being caused by genetics seems like a paradox: if male infertility has a genetic link, how is it passed from one generation to the next? The medical community is still learning a lot about how genetics may influence a man’s ability to become a biological father, but it has become increasingly clear that genetics can play a role for a significant number of men who struggle to achieve a pregnancy. For one, we have learned that genetic infertility can be “new” to the patient and not necessarily inherited from a parent. In addition, it has also become clear that male infertility can be inherited from a mother as male infertility genes have been found on the X (female) chromosome.
Dr. Paul Turek, a leading urologist and male infertility surgeon, continuously researches the effects that genes have on male fertility so that he may offer the best possible care and advice to his patients. He founded the country’s first genetic testing and counseling infertility program to help patients affected by this problem. With a comprehensive evaluation, Dr. Turek can identify whether genetics are a factor in a man’s infertility struggles and customize a treatment plan that best addresses these issues.
Overview
Among the 15% of couples who experience infertility, about 40% of the time the infertility is due to male “factors.” About half of male infertility cases are due to defined reasons, including varicocele, infection, hormone imbalances, exposures such as drugs or medications, x-rays, tobacco use and hot tubs, blockage of the reproductive tract ducts, and previous surgery that has left scarring.
Another cause of male infertility that has been underestimated in the past is genetic infertility. The reason for its increased importance is that our knowledge about genetics is growing quickly. Men who may have had unexplained infertility in the past may now be diagnosed with genetic causes thanks to recently available testing. In fact, this field is progressing so quickly that genetic infertility has already become one of the most commonly diagnosed reasons for male infertility.
Why does it matter if infertility has a genetic cause?

Developed in the early 1990’s, assisted reproduction in the form of IVF and ICSI (intracytoplasmic sperm injection) is a revolutionary laboratory technique in which a single sperm is placed directly inside an egg for fertilization. This technique has opened the door to fertility for men who formerly had few available treatment options, as it offers men who were previously considered severely infertile or sterile the possibility of fatherhood.
Because sperm used in ICSI sperm are chosen by laboratory technicians rather than nature, natural selection may be altered. Thus, along with this technology comes the possibility of passing on to a child the same genetic issues that may have caused the father’s infertility, or perhaps even more severe conditions.
Another reason to determine whether a man’s infertility is caused by genetics is because many of the classic treatments for infertility (such as varicocele repair or medications) will not help. In fact, Dr. Turek was one of the first to publish on this issue, showing that varicocele repair was not effective in improving fertility in men with genetic infertility.
Because he recognized these issues early on, Dr. Turek founded the first formal genetic counseling and testing program for infertility in the U.S. named the Program in the Genetics of Infertility (PROGENI) at UCSF in 1997. Dr. Turek’s program has helped over 2,000 patients at risk for genetic infertility to navigate the difficult decisions surrounding this condition.
Testing for Genetic Male Infertility
Men with infertility should be seen by a urologist for a thorough medical history, physical examination, and appropriate medical testing. If genetic infertility is a possibility, men can be offered appropriate genetic testing. The results are discussed with the care provider or a genetic counselor given the complex emotional and medical implications of the test results.
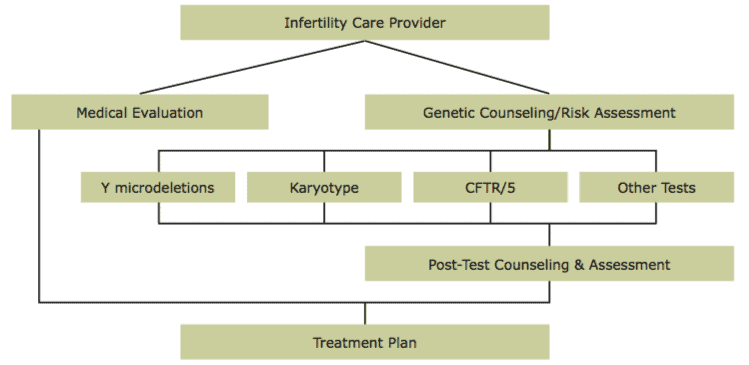
The approach taken early on by Dr. Turek is outlined in the chart below. Just like the medical diagnosis from a urologist or fertility specialist, information about family history plays a critical role in genetic risk assessment. This approach to genetic evaluation, termed non-prescriptive, has been the cornerstone of Dr. Turek’s critically acclaimed clinical program that now has over a dozen publications contributing to our current knowledge in the field.
It is important to note that a lack of family history of infertility or other medical problems does not eliminate or reduce the risk of genetic infertility. In fact, a family history review will often be unremarkable. However, family history can provide crucial supporting information toward making a genetic diagnosis (such as a family history of recurrent miscarriages or babies born with problems).
Dr. Turek has published that having a genetic counselor obtain family history information is much more accurate than simply giving patients a written questionnaire to fill out and bring to their visit. A genetic counselor can also discuss appropriate genetic testing options and review the test results in patients in a meaningful way.
When speaking to Dr. Turek or his genetic counselors about genetic testing, keep in mind that he or she does not tell patients what to do. Genetic counselors are trained to provide information, address questions and concerns, and support patients in the decision-making process. A genetic counselor does not assume which decisions are most appropriate for you.
Male Infertility Conditions That May Be Genetic
Among the various infertility diagnoses that men can receive, some are more commonly associated with genetic causes, such as:
- Nonobstructive azoospermia (no sperm count)
- Oligospermia (low sperm count)
- Congenital absence of the vas deferens.
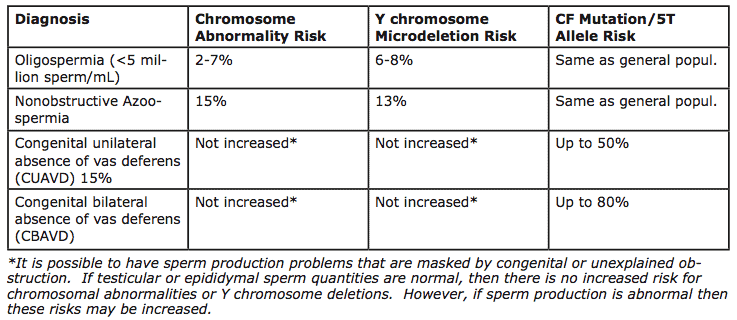
A list of some of the best-described causes of genetic male infertility and their frequencies and associated conditions are listed in Table 1.
Nonobstructive azoospermia
Nonobstructive azoospermia is defined as zero sperm count in the ejaculate due to an underlying sperm production problem within the testicles. This is quite different from obstructive azoospermia in which sperm production within the testes is normal, but there is a blockage in the reproductive tract ducts that prevents the sperm from leaving the body.
There can be changes in the levels of reproductive hormones, such as follicle stimulating hormone (FSH), observed with nonobstructive azoospermia. Most commonly, the FSH is elevated in this condition, which is an appropriate and safe hormone response of the pituitary gland to states of low or no sperm production.
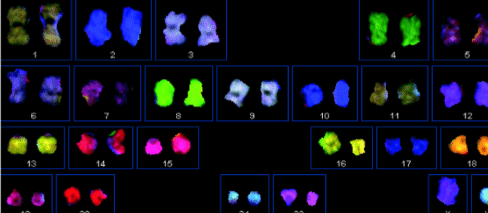
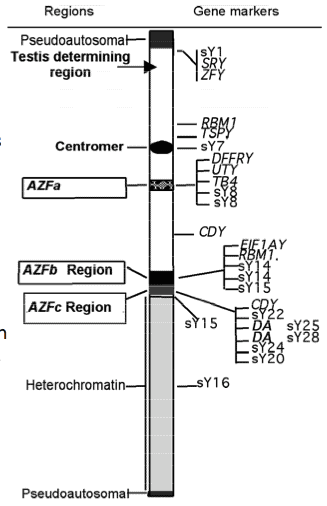
This diagnosis is associated with a 15% chance for having chromosome abnormalities (Figure 2) and a 13% chance for having gene regions missing on the Y chromosome (termed Y chromosome microdeletions, Figure 3). To detect these changes, blood tests are typically offered to men with nonobstructive azoospermia.
Oligospermia
Oligospermia that places men at risk for genetic infertility occurs when the ejaculate contains a sperm concentration of <5 million sperm/mL semen. Similar to nonobstructive azoospermia, this is most commonly due to an underlying sperm production problem.
With this diagnosis, there is a 2% risk for chromosome abnormalities and 6-8% risk of Y chromosome microdeletions. In general, the lower the sperm count, the higher the chance that a genetic cause is present. Again, the appropriate testing includes a karyotype and Y chromosome microdeletion analysis. Thus far, there are no established guidelines for applying these genetic tests in cases of low sperm motility (movement) or poor sperm morphology (shape).
Congenital absence of the vas deferens (CUAVD, CBAVD)
Congenital absence of the vas deferens is characterized by the malformation or absence of the ducts that allow sperm to pass from the testicles into the ejaculate and out of the body during ejaculation. The duct that is affected in this condition is the vas deferens. This is the same duct that is treated during a vasectomy, a procedure for men who want birth control. Men with this condition are essentially born with a “natural vasectomy.”
This congenital condition is associated with mutations and/or variations in the genes for cystic fibrosis (the CFTR gene), the most common genetic disease in the U.S. About 70-80% of cases where men are missing their vas deferens on both sides (CBAVD) are due to this condition, but the rate of finding a genetic mutation is much lower if the duct is missing on only one side (CAUVD). For most men with this condition who have a mutation in the cystic fibrosis gene, the missing vas deferens is the sole problem that results from this genetic change. That means they do not have the full spectrum of symptoms normally associated with cystic fibrosis.
Unexplained obstruction or blockage
A less common reason for men to have a zero sperm count (azoospermia) than nonobstructive azoospermia is obstructive azoospermia. In essence, this is an unexplained zero sperm count due to a blockage of the reproductive tract ducts leading from the testicle to the ejaculate. Blockages are usually found in the epididymis, but they can also be located in the vas deferens or ejaculatory ducts.
Most cases of obstructive azoospermia can be surgically repaired to promote natural fertility. However, a high proportion of these men (47%) have mutations in the cystic fibrosis gene (CFTR) or harbor variations in the CFTR gene, termed 5T alleles. As such, genetic counseling and testing is also important in these patients.
These conditions represent only the most common genetic conditions encountered when evaluating men for genetic infertility. For this reason, consider reading Dr. Turek’s published paper that discusses most of the currently understood syndromes and conditions that are associated with infertility. It is also important to remember that if all genetic test results return as normal, there is still a possibility that the infertility has a genetic cause, as currently used tests may not be advanced enough to detect all possible genetic issues these cases.
Chromosome Abnormality
If a man has a chromosome abnormality known to impair fertility, then it may the raise the risk for a resulting pregnancy to miscarry or his children to be born with birth defects or mental impairment. This occurs because the children inherit an imbalance in chromosome material from their biological father.
A genetic counselor can provide more detailed information about specific potential risks and offer other resources for individuals who have been diagnosed with a chromosome abnormality. There are also support organizations available to help men with genetic diagnoses and their partners cope with the impact of this information. Some couples find it helpful to talk to others in similar circumstances.
Y Chromosome Microdeletion
If a man is diagnosed with a Y chromosome deletion, then he will pass on that Y chromosome deletion to any son he conceives. (To his daughters, he will pass on his X chromosome, instead of the Y chromosome). It is assumed that any son inheriting a Y chromosome deletion from his father will also be infertile, although it is unclear whether the type and severity of the infertility will be different from the father’s.
So far, there have only been a few reports of sons born to fathers with Y chromosome deletions after conception by assisted reproduction. As expected, there has not been an increase in the rate of birth defects or other problems for these boys. Because of the small sample size and the age of these subjects, fertility issues have yet to be evaluated in these boys.
CFTR Mutations
Transmission of CFTR mutations in cases of infertility due to congenital absence of the vas deferens is somewhat more complex than either Y microdeletions or a chromosome abnormality. This is because there are over 2000 described mutations in the CFTR gene, and the impact of mutations differs depending on which one is present. In general, the partner of an affected man should be tested as well, so that the residual risk of a child having either congenital absence of the vas deferens or full-blown cystic fibrosis can be estimated.
Seek Treatments for Genetic-Based Male Infertility Problems at The Turek Clinic
Ultimately, the most appropriate treatments for achieving a pregnancy depend on the diagnosis from genetic testing. Some men can still conceive a child with minimal risk to offspring, while other men may need to examine these risks and probabilities in more detail before conceiving. Either way, it’s a good idea to have a leading infertility expert and professional counselor to help guide you through this process. Please schedule a consultation with Dr. Turek to finally receive the answers to all your infertility questions.









