Vasectomy Reversal Techniques

Dr. Turek utilizes a number of vasectomy reversal techniques depending on the individual needs of each patient. If you are ready to schedule a consultation to learn more about your vasectomy reversal options, please contact The Turek Clinic today.
Vasovasostomy
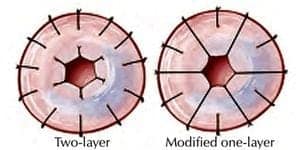
Figure 1. Suture Placement for Vasovasostomy Techniques
There are two microsurgical approaches available for a vasovasostomy and vasectomy reversal specialist, Dr. Paul Turek, has extensive experience with both. One surgical approach is the modified 1-layer connection (anastomosis) and the other is a formal, two-layer anastomosis. The technical differences in suture placement are shown in Figure 1.

For this discussion, we will outline the 2-layer method. Using the technique, the freshened ends of the vas deferens are brought closer together by placing small sutures in the surrounding tissue. Once the two ends face each other, the formal microsurgical connection is begun. The connection begins with the backwall, then the inner layer, both held together with six sutures around the circumference of the vas deferens. Once the entire inner and outer layers have been connected, larger sutures are places around the vas deferens to create a tension-free vasal connection. The vas deferens is then placed back into the scrotum and local anesthesia is given to ensure a pain-free recovery.
Mucosa-Mucosa Epididymovastomy

Dr. Turek uses two epididymovasostomy procedures, the mucosa-mucosa method and the invagination method. In the mucosa-to-mucosa, end-to-side method of vasectomy reversal, an opened epididymal tubule is microsurgically connected to the cut end of the vas deferens with up to six simple sutures. This “inner” layer is supported with an “outer” layer of radial sutures to strengthen the epididymovasostomy.
Invagination Epididymovastomy
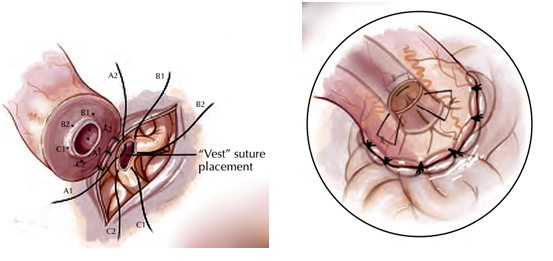
Recently, the idea of end-to-side connections (also termed mucosa-to-mucosa) has been challenged. A new technique, termed invagination epididymovasostomy, that does not use the edge-to-edge connection, has become popular over the last several years. The essential difference between this new technique and the edge-to-edge technique for vasectomy reversal surgery is that the epididymal tubule edge is not sutured to the vas deferens edge. Instead the sutures are placed such that the epididymal tubule is carefully pulled into the hole of the vas deferens or invaginated into it. This new technique uses fewer sutures and appears to be a more leak-free anastomosis than the edge-to-edge approach to vasectomy reversal surgery. Dr. Turek was an early adopter of the invagination epididymovasostomy and uses this new vasectomy reversal technique as much as possible.
After either method of epididymovasostomy, Dr. Turek limits physical activity for 3-4 weeks. He occasionally places small, painless rubber drains in the scrotum during the procedure to minimize any potentially harmful collections of fluid or blood. These drains are typically removed the day after your epididymovasostomy procedure.
Magnifying Lubricants
A new vasectomy reversal technique that was invented by Dr. Turek uses a novel lubricant to make vasectomy reversals easier to perform. This new technique involves a safe, nonreactive lubricating bulking agent called Viscoat® that has been used by ophthalmologists for years in delicate eye surgery cases.
Dr. Turek has found that when this new technique is used in vasectomy reversal cases, this substance helps make the vas deferens lumen larger for easier suture placement and magnifies the microsurgical view of the vas deferens lumen. It also helps visualize the connection without the need for cautery that can damage tissue. And this benefit comes without any loss of patency rate when compared to vasectomy reversal cases in which Viscoat is not used. This magnifying lubricant has become an important new technique or “tool” in Dr. Turek’s microsurgery cases and is an example of how a master microsurgeon is constantly looking for ways to improve outcomes after vasectomy reversal.









