Male Fertility Preservation

Most children and young adults treated for cancer can expect to be cured. In fact, 70% of children with cancer survive their malignancies. Among adult survivors, future fertility is often the key quality of life issue on their minds once the threat of cancer has passed. The Turek Clinic understands the importance of preserving and restoring male fertility and has developed a comprehensive, streamlined evaluation for affected men.
It’s bad enough that cancer puts you face to face with your own mortality, but it often also deals a mortal blow to the dream of fatherhood. This motivates me to do everything I can to help.
– Dr. Paul Turek
Evaluating Men For Fertility Preservation

The evaluation of men for fertility preservation is a quick but methodical process performed in the office and is similar to the male infertility evaluation. At The Turek Clinic, patients interested in fertility preservation are scheduled and seen without delay, as time constraints are usually present. The office visit involves taking a thorough personal history and physical examination, obtaining a high quality semen analysis with assessment of a centrifuged pellet for sperm, and a blood draw for reproductive hormones. Based on the findings from this evaluation and the timeline imposed by cancer treatment, an individually tailored plan for fertility preservation or restoration is proposed.
Effects of Cancer on Male Fertility
Fertility in men with cancer can be compromised by both the disease and its treatment. For example, low or no ejaculated sperm counts are detected in 60% of men with Hodgkin disease, an effect thought to be due to fever and general symptoms associated with the illness. Likewise, 50% of men with testis cancer have low sperm counts at the time of diagnosis, in many cases because the tumor is hormonally active. In addition, cancer treatment has profound effects on fertility, as sperm production involves rapid cell division and is therefore exquisitely sensitive to treatments designed to kill equally rapidly dividing cancer cells. Table 1 lists the most common chemotherapy agents used for cancer treatment and their effects on sperm production.
Table 1. Effect of Various Chemotherapy Agents On Male Fertility.
| Agent | Effect on Testis | Recoverability | Recovery Time |
|---|---|---|---|
| Mechlo1rethamine | Severe | Poor | >2-5 years |
| Cyclophosphamide | Severe | Poor | 1-5 years |
| Chlorambucil | Severe | Poor | 3-5 years |
| Methotrexate | Minimal | Good | 6-12 months |
| Cytosine arabinoside | Moderate | Good | 6-12 months |
| 6-Mercatopurine | Moderate | Good | 6-12 months |
| Thioguanine | Moderate | Good | 9 months |
| Vincristine | Moderate | Good | 6-12 months |
| Pednisone | Moderate | Good | 6 months |
| Androgens | Moderate | Good | 6-12 months |
| Estrogens | Severe | Good | 6-12 months |
| Doxorubicin | Moderate | Good | 1 year |
| Procarbazine | Severe | Poor | >2-5 years |
| Cisplatin | Moderate | Good | 1-2 years |
| Nitrogen mustard, vincristine, procarbazine, and prednisone | Severe | Very Poor | >2-5 years |
| Cyclophosphamide, vincristine, procarbazine, and prednisone | Moderate | Moderate | 3 years |
| Doxorubicin, bleomycin, vinblastine and decarbazine | Moderate | Moderate | 1-4 years |
| Cisplatin, etoposide, and bleomycin | Moderate | Good | 1-2 years |
| Vinblastine, bleomycin, and cisplatin | Moderate | Good | 1-2 years |
Similarly, Table 2 demonstrates how sensitive the testicles are to exposure from radiation therapy.
Table 2. The Effect of Radiation Therapy on Sperm Counts
| Radiation Dose | Equivalent To | Effect on Sperm Counts |
|---|---|---|
| 15 cGy | 150 chest X-rays | Significantly lowers sperm count |
| 50 cGy | 500 chest X-rays | Causes complete loss of sperm counts (azoospermia); usually only temporary |
| 78 cGy | 780 chest X-rays | Typical amount of radiation “scatter” to the testicles with treatment given below the chest for cancer with the use of gonadal shielding |
| 500 cGy | 5000 chest X-rays | Causes complete loss of sperm counts (azoospermia); usually permanent |
| 632 cGy | 6320 chest X-rays | Typical amount of radiation “scatter” to the testicles with treatment given to the pelvis without gonadal shielding |
Surgery needed to cure cancer may not affect sperm production directly, but can impair erections and the ability to ejaculate and therefore make natural conception difficult. The kinds of surgical procedures that affect fertility are listed in Table 3.
Table 3. Surgical Treatments for Cancer that Can Affect Male Fertility
| Radical Orchiectomy | Removal of one or both testicles and associated structures. |
| Retroperitoneal Lymph Node Dissection (RPLND) | Removal of lymph nodes or cancer in the back of the abdomen |
| Pelvic Surgery | Removal of lymph nodes or cancer in the pelvic area, including the prostate. |
| Spinal Cord Surgery | Removal of cancer from the lower spinal cord |
Effects of Cancer on Offspring
Patients often wonder whether cancer treatments can affect the health of their offspring. One way of looking at this is to examine damage to sperm. In studies that have examined sperm chromosomes in patients receiving chemotherapy, it is clear that chromosomal abnormalities in sperm increase by five-fold when measured during chemotherapy compared to before treatment. This rate of chromosomal damage returns to baseline levels (pre-treatment) 100 days after chemotherapy ends. It is also clear that exposure to chemotherapy causes high levels of sperm DNA fragmentation that persists for up to a year after treatment.
These findings have led to the following recommendations:
- Sperm should not be banked while a patient is receiving chemotherapy
- Contraceptive intercourse is advised during chemotherapy treatment
- Fertility should not be considered until at least 6 months after chemotherapy finishes
Although there are measurable effects of cancer treatment on sperm, does this translate into having children with birth defects? Simply stated, numerous human fertility studies that have addressed this issue have not shown higher rates of birth defects in cancer survivors who conceive naturally compared to otherwise healthy men. Whether or not this is also true with conception using assisted reproduction has not been well studied as the technology is still young. However, Dr. Turek’s published research has shown that children conceived with IVF-ICSI using testicular sperm from men who had received chemotherapy did not show higher rates of birth defects than that expected with natural conception.
Methods of Fertility Preservation Before Cancer Treatment
Gonadal Shielding
Radiation therapy affects organs far away from the intended target by “leakage” through machine shielding, by “scatter” from the radiation beam, or from radiation “scatter” within the patient. Gonadal shielding can prevent 99% of the “leaked” and beam scatter radiation to the testicles and should be employed for all men receiving radiation below the chest (infradiaphramatic) for cancer.
Sperm Cryopreservation or Banking
The single best way to preserve fertility in patients who undergo cancer treatment is banking sperm before treatment. This is performed on ejaculated semen after a routine semen analysis and therefore requires there to be sperm in the ejaculate. The semen is placed in plastic vials or “straws” and is mixed with cryoprotectants (egg yolk-citrate buffer) and frozen in liquid nitrogen (-196° C). When needed, straws are thawed, washed free of cryoprotectants and then used for either intrauterine insemination (IUI) or in vitro fertilization (IVF). If semen quality is normal prior to sperm banking, a 40% to 60% recovery rate of usable (motile) sperm is generally obtained. With impaired semen quality, rates of usable sperm recovery are lower. The ability of sperm to recover after freezing and thawing is generally independent of the length of time that the sperm is banked. Based on this information and Dr. Turek’s experience with cancer patients, The Turek Clinic makes the following recommendations for sperm banking:
- Semen quality and sperm counts do not have to be normal to be banked. Any semen sample that shows motile or viable sperm should be banked, as even the poorest quality sample (with as few as 1-50 motile sperm) can be used with IVF-ICSI to conceive.
- Even if ejaculated semen has no sperm, sperm retrieval techniques can be used before cancer treatment to bank sperm for future use (see below).
- To decide on how many semen samples should be banked, the following information should be considered. As a general rule, a single ejaculated semen sample of normal quality will provide 2 to 3 attempts at conception by intrauterine insemination (IUI) after thawing. Couples should plan on 6 monthly IUI attempts to conceive each child (i.e. 2-3 banked ejaculates of normal quality).
Electroejaculation
For men who are unable to provide an ejaculate before cancer treatment either because they are too ill or due to underlying neurologic issues, electroejaculation can be considered. Performed routinely at The Turek Clinic, this technique obtains the ejaculate through normal channels by electrically stimulating the spinal reflex that controls ejaculation. Although quick, the technique does require a light, general anesthesia to be successful. Collected ejaculated sperm is then washed and banked in routine fashion. When fertility is desired in the future, the banked sperm can be used with IUI or IVF, depending on initial semen quality and recovery after thawing.
Sperm Retrieval Techniques
In men who do not have sperm in the ejaculate (azoospermia) for sperm banking, it may be possible to retrieve and bank sperm from the reproductive tract before cancer treatment. Sources of sperm that can be retrieved include the vas deferens, epididymis, and testicle. If sperm production is normal, vas deferens (VASAL), epididymal (MESA, PESA) and testis sperm (TESA, TESE) retrievals are possible. With impaired sperm production, testis sperm (OncoTESE, Microdissection TESE) is the only source of sperm for banking. OncoTESE procedures can also be considered in teenage boys who are too young to ejaculate or who have not yet developed sperm in the ejaculate, as they may still have bankable sperm in the testicle. Finally, it can also be considered as a way to preserve testis stem cells from non-sperm bearing testis tissue in prepubertal boys, although this is still considered experimental. These procedures can be performed with very short notice under local anesthesia (with intravenous sedation if desired) on a come-and-go basis. In addition, patient recovery is rapid and cancer treatment can be started within 1-2 days after sperm retrieval. Importantly, IVF-ICSI (as opposed to IUI) is generally required to conceive with retrieved sperm.
Testis-Sparing Surgery for Cancer
Dr. Turek has been an early proponent of organ-sparing testis surgery or partial orchiectomy as an alternative to radical orchiectomy in selected cases of testis cancer. The goal is to provide similar cure rates but also to preserve gonadal function. Although testosterone function may be well-preserved with this approach, there is also the potential for fertility preservation. These techniques are most appropriate in men with cancer in a solitary testis or in men with testis cancer on both sides.
Methods of Fertility Restoration After Cancer Treatment

Bladder Harvest
For many men with a “dry ejaculate” after pelvic or retroperitoneal cancer surgery, usable sperm can be obtained from the bladder. Termed retrograde ejaculation, this problem is diagnosed by finding sperm in the post-ejaculate voided urine. Initially, a trial of medication can be used to convert men to ejaculate normally. For those who fail medication, bladder harvesting techniques can be used to retrieve sperm from the bladder for use with IUI or IVF for conception. A bladder harvest involves placing a small catheter in the bladder, draining the urine that is toxic to sperm, and replacing it with sterile fluid that supports sperm motility. After removal of the catheter, the patient ejaculates and then “urinates” the fluid and sperm from the bladder which is then washed for IUI or IVF, depending on sample quality.
Electroejaculation
The absence of sperm in the voided bladder urine after ejaculation indicates more extensive damage to the autonomic nerves, and is termed “anejaculation.” In the vast majority of these men, electroejaculation, as described above, can obtain usable sperm for IUI or IVF.
Sperm Retrieval Techniques
In patients with anejaculation after cancer treatment, sperm aspiration from the reproductive tract is an alternative to electroejaculation for men to achieve paternity. It is important to realize, however, that in IVF-ICSI is generally required to achieve a pregnancy with retrieved sperm.
Sperm retrieval techniques are also the mainstay for fertility restoration in men who have impaired sperm production (testis failure) after chemotherapy or radiation treatment for cancer. Remarkably, as Dr. Turek has published, 55-60% of men without ejaculated sperm (non obstructive azoospermia) after cancer treatment can have “pockets” of usable sperm in the testicles. Given that sperm production is very low, it may vary geographically within the testis, making a “blind” testis biopsy an inaccurate method to either diagnose or extract sperm. Several sperm retrieval strategies have been developed to find sperm in the testis of men after cancer treatment, including Dr. Turek’s Sperm Mapping™ technique using fine needle aspiration (FNA) that helps detect and locate mature sperm in the testis after cancer treatment.
The Future of Fertility Preservation
Protecting Sperm Production
Chemotherapy and radiation therapy impairs male fertility by destroying valuable testicular stem cells that are constantly and rapidly dividing to make sperm. To prevent the destruction of these delicate stem cells before cancer treatment, attempts have been made in animals to “slow down” or “suspend” testis stem cells from dividing by reducing the hormonal drive to the testis to make sperm. If done prior to chemotherapy, the testis might be protected from the devastating effects of chemotherapy on rapidly dividing testis stem cells. Various hormonal regimens have been studied in animals, including estrogens, androgens, anti-androgens, GnRH agonists, and GnRH and these studies have met with varying levels of success. In the few studies performed in humans, the results have been largely disappointing. However, as this research is refined, it is conceivable that hormonal manipulation may emerge as a workable form of testis protective therapy.
Germ Cell Transplantation
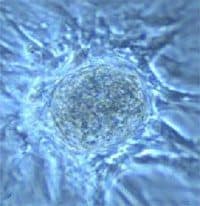
A very exciting innovation in the understanding of how a sperm is made may also have practical application to restore sperm production after cancer treatment. Termed “germ cell transplantation,” this technique has the greatest value in preserving fertility in pre-pubertal or teenage boys who are unable to ejaculate and bank sperm before sterilizing cancer treatment. The technique involves harvesting testis tissue containing testis stem cells (but not sperm) before cancer treatment through a biopsy and banking the tissue as described above under Sperm Retrieval Techniques. Subsequently, the testis tissue containing the stem cells is thawed and transplanted back into the testicle after cancer treatment. Through this technique, the “sterilized” testicle is repopulated with testis stem cells that can produce ejaculated sperm in the future. Although its success has been demonstrated in many animal species over the last decade, germ cell transplantation has not been extensively studied in humans and is still experimental.
Testis Grafting
A variation on germ cell transplantation, testis grafting, involves the concept of placing previously banked and thawed testis tissue back into the patient under the skin instead of into the testicles. Obviously, sperm would not be ejaculated with this technique but sperm might be able to be retrieved from the “testis” in its new location. This technique has generated mature sperm and live births through IVF-ICSI from mouse, rabbit, pig and goat testis tissue that was reconstituted in mice. However, extensive human studies have not been performed to date.









