Semen Analysis in Los Angeles & San Francisco

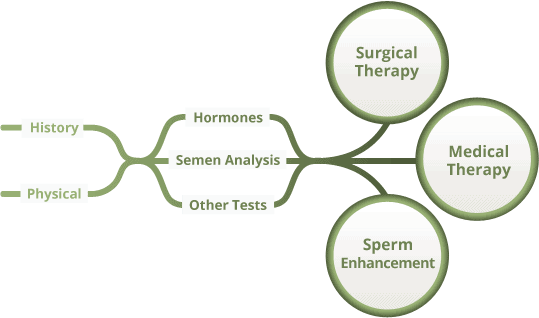
Traditionally, the health care response to a couple with infertility has been for the female partner to visit a gynecologist for evaluation. The male partner may or may not be asked to give a semen analysis (often called a “sperm test”). If the semen analysis is abnormal, couples are often shuttled straight to assisted reproduction for IUI or IVF, instead of examining (a) why the semen sample may be abnormal and (b) correcting the abnormal semen analysis and therefore the infertility. In the modern era of evidence-based care and cost-containment, this sequence of events is now inappropriate. Dr. Paul Turek is a renowned, board-certified doctor and male fertility specialist with an in-depth understanding of semen analysis biology and has a proven track record of helping couples to conceive. He recommends the methodical evaluation of male infertility to acquire 4 kinds of information (Figure 1 under Patient History). From there, a decision is made to pursue surgical or nonsurgical treatment. If neither is appropriate, assisted reproduction can be used to overcome even some of the severest forms of male infertility.
To learn more about male fertility evaluation and testing, please select one of the following topics. If you are ready to schedule a consultation with Dr. Turek, please request a consultation here.
Patient Medical History

To begin, Dr. Turek reviews your medical history, including recent fevers, illnesses, cancer, and infections, as well as prior surgeries such as orchidopexy, herniorrhaphy, trauma, open retroperitoneal, pelvic or bladder procedures, and prostate surgery. He also looks for a family or genetic history of cryptorchidism, midline defects, or hypogonadism, or a developmental history of hypospadias, congenital anomalies, and DES exposure. Use of medications including finasteride (Propecia), nitrofurantoin, sulfasalazine (and possibly other sulfa drugs), cimetidine, alpha-blockers, calcium channel blockers, allopurinol, and many other medications may also impact fertility.
Patient Social History
Medical ailments are not the only factors that warrant review in the fertility history. It is also helpful to take inventory of your social history since the habitual use of alcohol, tobacco, recreational drugs, and anabolic steroids can all hurt sperm production. Dr. Turek published the first research study to convincingly demonstrate that hot tubs and baths can have a major impact on semen quality, so that is considered as well.
Dr. Turek reviews your sexual history, paying special attention to the timing of intercourse and use of spermicidal lubricants. Finally, an occupational history is important to determine exposure to ionizing radiation, chronic heat, dyes, pesticides, herbicides, and heavy minerals (lead, cadmium, and mercury).
In most cases, adverse exposures discovered during the patient history-taking process are reversible. After identifying these factors, you may be advised to modify or discontinue certain habits or medications to improve your fertility.
Key Points for Patients:

- Bring any information you may have from prior evaluations. Collect prior lab reports and bring them with you to the initial visit. Semen analyses or hormone testing can help
- avoid duplicating tests
- give further evidence of a male infertility problem
- show semen quality trends over time to help identify root causes
- Bring your female partner. Dr. Turek is very interested in her history of prior pregnancies, how regular her cycles and menstrual flow are, and whether intercourse was “timed” or simply unprotected. The most important piece of information about her is her age, as fertility in women declines after age 35 and is almost certainly decreased at 40.
Physical Examination
During a physical examination, Dr. Turek assesses blood pressure, height, weight, and body mass, as well a body habitus including gynecomastia and obesity. The testes are evaluated for size, consistency, and irregularities. If the epididymides are swollen or tender, that can indicate an infection or obstruction.
Careful palpation of each vas deferens can show that they are missing, abnormal, or inflamed. The spermatic cords above the testes should be felt to check for asymmetry, which may be a sign of varicocele or a lipoma. Finally, a rectal exam evaluates the health of the prostate, paying attention for infections, cysts, or dilated seminal vesicles.
Semen Analysis (“Sperm Test”)
While it is not a true assessment of actual fertility, the semen analysis, if irregular, may suggest that the odds of achieving fertility are statistically low. A semen analysis measures ejaculate volume, sperm concentration, as well as motility; among these, motility correlates best with fertility. Two well-performed semen analyses can often lead to a diagnosis or inform Dr. Turek’s treatment recommendations. Normal values for the semen analysis are found in Table 1.
Table 1. Semen analysis-W.H.O. 2010 reference ranges
Also: No agglutination (clumping), white cells, or increased viscosity
Sperm Morphology
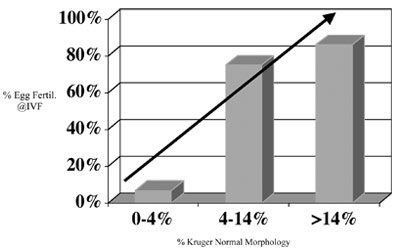
Morphology is the evaluation of the various shapes of sperm. Sperm are designated normal or abnormal based on a comprehensive list of criteria. Sperm morphology has primarily been helpful in identifying the sperm’s ability to penetrate and fertilize eggs in the setting of in vitro fertilization (IVF) (Figure 2).
So far, studies have not convincingly correlated sperm morphology with couples’ ability to conceive, either by sexual intercourse or intrauterine insemination (IUI). Sperm morphology is also a sensitive indicator of testicular health since the shape of sperm is determined during the process of sperm production in the testis. The main function of morphology in male evaluation is to complement the semen analysis data and better estimate the chances of fertility.
Tips for Patients:
- Choose a reputable semen analysis lab known for producing high-quality evaluations and reports. Labs associated with fertility clinics are generally good at performing semen analyses.
- Follow instructions closely since the collection technique can affect the quality of the semen.
- Do not ejaculate for about three days prior to producing your semen sample. Abstaining for a shorter or longer period can produce an artificially inflated/deflated sperm concentration.
- Only use sterile containers to collect your semen.
- Avoid using lubricants and condoms during the collection of your sample since they may contain spermicide.
- Keep your sample at body temperature while transporting it. Be sure to deliver it to the lab within an hour of producing the sample.
Hormone Tests
Testing pituitary-gonadal hormones can provide valuable information on the state of sperm production since abnormalities of these hormones may cause infertility. The standard hormone test evaluates FSH (follicle-stimulating hormone), testosterone, LH (luteinizing hormone), and prolactin. Estradiol levels may also be included for infertile men with soft testicles and a sperm concentration less than 10 x 106 sperm/mL. The more common patterns of hormonal disorders seen with infertility are in Table 2.
Table 2. Characteristic hormone profiles in infertile men.
Key Points for Patients
Hormone levels should be measured if:
- Sperm concentration is less than 10 x 106 sperm/mL
- There is impaired sexual function (erectile dysfunction, low libido)
- There are exam findings of a specific hormone disorder (i.e., thyroid).
Further Male Infertility Testing
Many other tests are available to help evaluate male infertility if the 4-point evaluation fails to find a diagnosis. Dr. Turek does not order further tests on a whim, firmly believing in only ordering tests if they may change the way the patient is managed. These tests include:
- Seminal Fructose and Post Ejaculate Urinalysis: Fructose is normally present in the ejaculate. If absent, or if the pH in the ejaculate is low, then the seminal vesicles may be missing or obstructed. A post-ejaculate urinalysis (PEU) is a microscopic inspection of the first voided urine after ejaculation for sperm. Retrograde ejaculation is diagnosed in this manner.
- Semen Leukocyte Analysis: If “round” cells are found in a standard semen analysis in addition to normal sperm with tails, they may be either spermatocytes (immature sperm) or leukocytes (white blood cells). This test determines which type of rounded cell is present since the treatment for each is different.
- Sperm DNA Fragmentation Assay: When sperm DNA fragments, this can impact fertility. Fertile men almost never have fragmented sperm DNA, whereas about 5-20% of infertile men have this problem. Sperm can be tested for fragmented DNA with COMET and TUNEL assays. The good news is that sperm DNA fragmentation is often reversible.
- Scrotal Doppler Ultrasound: A high-frequency (10mHz), non-invasive ultrasound of the scrotum has become a mainstay in the evaluation of testicular and scrotal lesions. Most commonly, Dr Turek will order this to look for clinically suspicious varicoceles.
- Transrectal Ultrasound (TRUS): A high frequency (5-7mHz) transrectal ultrasound offers superb imaging of the prostate, seminal vesicles, and ejaculatory ducts. This is a first-line method of diagnosing ejaculatory duct obstruction.
- CT Scan/MRI Pelvis: Since the advent of TRUS, these tests have become rarer for fertility purposes. One of the main reasons Dr. Turek may order this study today is to further evaluate a patient with an isolated right varicocele.
- Karyotyping: A chromosomal analysis is performed in men with low (less than 5 million) or no sperm in the ejaculate. For more information, please read about genetic infertility.
- Y Chromosome Analysis: It has become apparent that up to 8% of men with low sperm counts and 15% of men with no sperm counts may be missing small portions of the Y chromosome, termed Y–microdeletions. For more information, please read about genetic infertility.
Key Points for Patients:
Additional tests should only be ordered if it would do either of the following:
- Delineate treatable problems
- Define life-threatening problems
Meet with a Leading Male Infertility Specialist
Although it is wise to choose a doctor who offers such a wide range of tests, it is wiser still to choose a doctor who is selective in the tests he performs to identify fertility problems. It is costly and time-consuming to go through a battery of tests that may offer no relevant information in your and your partner’s quest to become parents. While Dr. Turek is committed to exploring every avenue necessary to achieve your fertility goals, in many cases preliminary analyses can reveal solutions that make other steps unnecessary. This is part of the wisdom he imparts to every infertility case. To undergo a semen analysis with Dr. Turek, please schedule a consultation.