Testis or Testicular Biopsy in Los Angeles & San Francisco
A testis biopsy is helpful in many cases of azoospermia. If an evaluation of azoospermia is not clearly showing whether there is a problem with sperm production or one of a blockage in the ducts of the reproductive tract, then the next step is to examine the testis itself and assess sperm production.
This can be done in several ways, but the classic approach is to perform a testis biopsy under local anesthesia. This allows for the direct inspection of a small piece of testis tissue to determine whether sperm production is normal or not. Testicular tissue contains
- sperm-producing cells that are found in tubules called seminiferous tubules, and
- cells between the tubules that are called interstitial or Leydig cells.
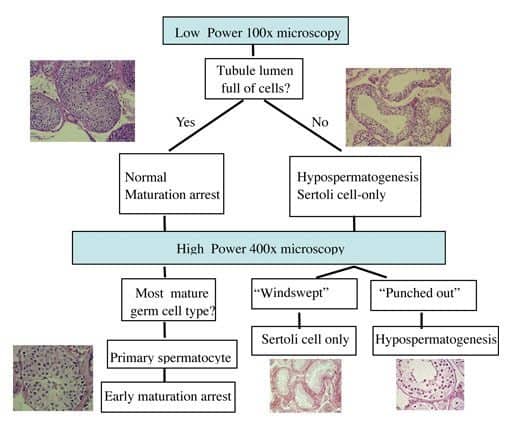
The Leydig cells are the major hormone-producing cells. The biopsied tissue is specially stained and examined microscopically for both cell types by a pathologist. If it shows that sperm production is normal, then a blockage exists in the system, usually beyond the testis. Remember that a biopsy does not tell us where the obstruction is located within the system. The most common testis biopsy patterns observed in a testis biopsy specimen are listed below. Dr Turek has created a systematic way to interpret the testis biopsy that he has taught others for years to decide what pattern is present (see figure below).
Testis Biopsy Result Patterns
Normal
The testis architecture and sperm production look entirely normal. This means that an absence of sperm in the ejaculate is due to an obstruction or absence of the ducts leading from the testicle to the penis.
Maturation Arrest
Sperm are made from early germ cells that develop within the testicle. The process of sperm maturation can be interrupted at several levels and can result in several “arrest” patterns. If the halt in development occurs early in the process of sperm maturation, the prognosis is worse.
Hypospermatogenesis
In this pattern, all of the elements of sperm production are present, but there are fewer of them than normal. This will generally result in lower numbers of sperm in the ejaculate.
Germ Cell Absence or Aplasia
This pattern occurs when there is no sperm found in the testicular biopsy. When there is no definite reason for this lack of germ cells and sperm, it can also be termed ‘Sertoli Cell-Only Syndrome’.
Other
Other abnormalities can be detected by examining a testis biopsy, including evidence of previous infection within the testis and abnormalities of the Leydig or interstitial cells. Occasionally, testis cancer can be detected, but this is a rare (less than 1%) finding in the U.S.
Limitations
In Dr. Turek’s experience, the testis biopsy has several limitations. For one, it is invasive. Second, it only provides information on the area that is biopsied and tells us nothing about sperm production in the rest of the testis. Third, how clinicians read the biopsies varies widely, making the interpretation unclear, a fact that does not help the patient. In fact, Dr Turek has published on this issue of how testis biopsy interpretations vary in a series of testis biopsies from patients who had had the biopsy procedure done before they consulted with him. In this study, he compared his interpretation of the biopsies from patients to the readings made by the pathologists from the community in which the biopsies were performed. He found that in 40% of cases, the interpretation that he made was different from the pathologist’s interpretation and that in 25% of cases, patient care was altered dramatically as a result of his re-review. An example of a significant alteration in care is a biopsy in which the community pathologist read as having no sperm but Dr. Turek’s reading suggested that there were sperm. For these reasons, the testis biopsy currently plays a limited role in the cutting edge care of azoospermic men. In addition, this is why Dr. Turek offers to re-review the testis biopsy slides that are sent to him as part of his Second Opinion Clinic.
Testicular Biopsy Results Interpretation
Testis Biopsy Alternatives
Because of the recognized limitations of the testis biopsy, about 15 years ago Dr. Turek pioneered a nonsurgical, less invasive alternative to the testis biopsy that is termed fine needle aspiration (FNA) “mapping” for men with azoospermia. FNA mapping is also known as sperm mapping™ or testicular mapping. He has performed over 1200 cases and testicular mapping is now popular throughout the world. More about testicular mapping.
Testicular Biopsy FAQs
Can a testicular biopsy be repeated?
Yes. Repeating a biopsy may be necessary if the initial sample was inconclusive. However, biopsies are invasive procedures, and repeated biopsies carry a small but increased risk of scarring and lowering of testosterone levels. Because of this, specialists like Dr. Turek prefer less invasive alternatives such as testicular mapping to gather good information instead of another biopsy.
Will a testicular biopsy affect my fertility or testosterone levels?
In most men, a single biopsy does not significantly impact testosterone production or fertility. Only a very small piece of tissue is removed, which usually has no measurable effect on testicular function. However, repeated, multiple or large biopsies may increase the risk of lowering male hormone production or scarring within the testis. This is why biopsies are best done by an experienced reproductive urologist who can minimize risk while maximizing diagnostic value.
How should I prepare for a testicular biopsy?
Preparation is straightforward. Patients are usually advised to avoid blood-thinning medications such as aspirin or ibuprofen for several days beforehand to reduce bleeding risk. On the day of the procedure, the scrotum is cleaned and local anesthesia is given. Some men may also be given a sedative to help with relaxation. Loose-fitting clothing and supportive underwear are recommended to wear home after the biopsy to minimize discomfort.
How soon will I get results from a testicular biopsy?
As testis biopsy specimens are preserved, stained and reviewed by expert pathologists, the results generally take a week, though timing can vary depending on the laboratory. The information obtained from a biopsy is generally more accurate than when sent to an IVF laboratory to look for sperm as staining the sample allows for a more precise identification of sperm than is possible with unstained fresh specimens. The final report provides detailed information on sperm production patterns and helps guide the next steps for fertility treatment.
Will insurance cover a testicular biopsy?
Coverage depends on the reason for the biopsy and your insurance plan. When the biopsy is ordered to evaluate azoospermia (absence of sperm) or to help diagnose infertility, some insurers may cover the cost. Others may classify it under fertility services, which are not always included in benefits. We recommend verifying coverage with your provider in advance; Dr. Turek’s team can assist with insurance questions and provide cost estimates.
Should I anticipate any recovery time?
Yes, but recovery is typically short. Most men return to desk work or light activity within one to two days. Strenuous exercise, heavy lifting, or sexual activity should be avoided for one week to allow the biopsy site to heal. Swelling and soreness are common but usually mild and temporary.
What are the alternatives to a testicular biopsy?
In some cases, alternatives like fine-needle aspiration (FNA) or testicular sperm mapping may provide similar information without requiring an incision. These minimally invasive options allow specialists to sample multiple areas of the testicle with far less trauma, helping to locate sperm for assisted reproduction. The choice between biopsy and alternatives depends on your specific diagnosis and the expertise and experience of your medical provider
Schedule a Testicular Biopsy Consultation
If you have recently been diagnosed with azoospermia and would like to learn more about the testicular biopsy procedure, schedule an appointment with Dr. Paul Turek at The Turek Clinic. Offices located in Los Angeles and San Francisco.
References:
- Cooperberg MR, Chi T, Jad A, Cha I, and PJ Turek. Fertil Steril 2005; 84: 672-7.









