Male Spermatogenesis in Los Angeles & San Francisco, CA
The male reproductive tract is an intricate system of tubes that can be difficult for someone without a medical background to fully comprehend. Nevertheless, for men who are grappling with a fertility issue, having a basic understanding of how sperm is created and released can be useful as many therapies aim to improve upon the process. To help educate his patients and other men who have been unsuccessful in their quest to become a father, renowned fertility specialist Dr. Paul Turek describes the basics on sperm and sperm production (spermatogenesis) and then discusses several obstacles men can face.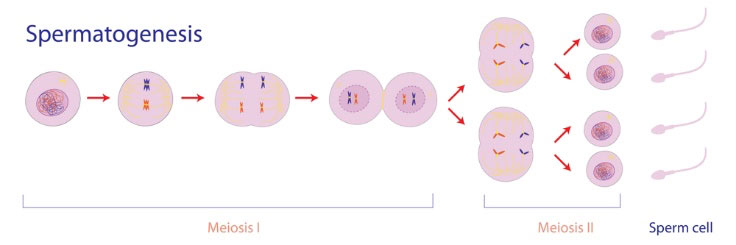
Human Sperm Production
Sperm Production Process
The male genitalia consist of the scrotum, which houses the testicles and associated ducts (the epididymis and vas deferens), and the penis (Figure 2). The testes are covered by a tough, white, fibrous layer called the tunica albuginea, which extends inward and divides the testis into 200 to 300 lobules. Sperm production occurs in the long and tightly coiled seminiferous tubules that are located in each of these lobules. Sertoli cells line the seminiferous tubules and serve as nurse cells to provide essential nutrients to sperm. In the absence of spermatogenesis, only Sertoli cells are seen on microscopic inspection of a testicular biopsy. Another important cell type within the testis are Leydig cells, which make testosterone, the essential male hormone. Testosterone is responsible for normal male secondary sex characteristic development, libido or sex drive and normal erections. Testosterone is also important for sperm production, as levels of this hormone are 50 fold higher within the testis as in the blood.
How Sperm is Made
Within the adult testicle, there is 700 feet of tubing, termed seminiferous tubules, within which sperm is made. Sperm is made from precursor cells termed germ cells that give rise to approximately 120 million sperm daily in a process termed spermatogenesis that takes approximately 64 days in humans. This is equivalent to making about 1200 sperm per heartbeat. Within the seminiferous tubule, germ cells are arranged in a highly ordered sequence from outside to inside. Lining the tubules, there are adult testis stem cells that begin the process of sperm production. Overall there are 13 recognizable germ cell types in the human testis: dark type A spermatogonia (Ad); pale type A spermatogonia (Ap); type B spermatogonia (B); preleptotene (R), leptotene (L), zygotene (z) and pachytene primary spermatocytes (p); secondary spermatocytes (II); and Sa, Sb, Sc, Sd1, and Sd2 spermatids. Despite the high volume production of sperm, quality control checkpoints exist throughout the sperm production process to ensure the biological and genetic integrity of ejaculated sperm.
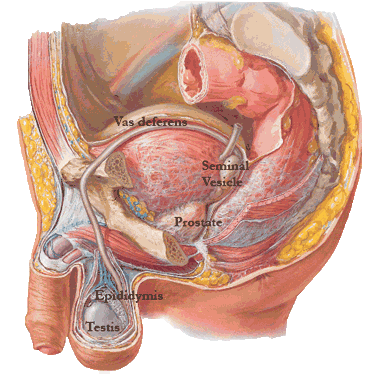
It has long been believed that sperm take 90 days (3 months) to be made and ejaculated. Dr. Turek recently discovered and published that in fact this time frame is actually much shorter. Sperm develop in the testicles for 50-60 days and are then excreted into the coiled ducts of the epididymis and complete their maturation for another 14 days. Sperm waiting to be ejaculated remain in the epididymis, near the bottom of the scrotum. At ejaculation, sperm are propelled through the vas deferens within the spermatic cord and into the abdominal cavity and join the seminal vesicles, which add alkaline fluid that helps to support sperm. The ejaculate consists of fluid from 3 sources: the vas deferens (sperm fraction), the seminal vesicles, and the prostate. The seminal vesicle fluid makes 80% of the total semen volume, the vas deferens 10% and the prostate gland another 10%. This mixture of semen then exits the penis during ejaculation.
What is a Sperm?
The spermatozoon is a remarkably complex metabolic, locomotive and genetic machine. It is approximately 60 microns in length and is divided into 3 sections: head, neck and tail. The oval sperm head consists of a nucleus containing the highly compacted DNA, and an acrosome that contains the enzymes required for penetration of the egg shell for fertilization. The neck maintains the connection between the sperm head and tail and consists of the connecting piece and proximal centriole. The tail harbors the midpiece, principle piece and endpiece. The tail midpiece contains the axoneme or engine of the sperm and the mitochondrial sheath, the source of energy for movement. Physiologically, the sperm axoneme is the true motor assembly and requires 200-300 proteins to function. Among these, the microtubules are the best-understood components. Sperm microtubules are arranged in the classic “9+2” pattern of 9 outer doublets encircling an inner central doublet. Defects in the sperm axoneme are well-recognized causes of ciliary dyskinesias that are routinely associated with infertility.
Spermatogenesis-Related Problems

Common problems that men face related to the production or transport of sperm include:
- Obstructive azoospermia: A physical blockage in the male reproductive tract that stops sperm before it is released in the ejaculate.
- Non-obstructive azoospermia: A complete lack of sperm in ejaculate that is due to a sperm production issue rather than an obstruction or blockage.
- Hormonal imbalance: Abnormally low or high levels of reproductive hormones, such as testosterone or prolactin, that can disrupt the normal production of sperm.
- Varicocele: Enlarged veins in the scrotum that overheat the testicles and impair sperm production.
- Asthenospermia: Men who have a normal sperm count but show poor sperm “motility” (movement). This is a very significant cause of infertility as sperm are less likely to reach, find, penetrate, and fertilize the egg.
- Teratospermia: Men who have normal sperm counts but irregularly shaped sperm. This can also be a significant cause of infertility as sperm have difficulty reaching, penetrating, and fertilizing an egg.
- Testicular problems: Chemotherapy, hot baths, and some medications can damage the testes in such a way that sperm production is lowered which reduces ejaculated sperm counts.
Treatments for Resolving Sperm Production Problems
Dr. Turek customizes treatments for his patients so that they can fulfill their goal of becoming parents. Treatment options include:
- Surgery can either unblock an obstruction so that sperm can be released into the ejaculate or correct varicoceles to reduce the temperature in the testicles for improved sperm production.
- Medication or hormone replacement therapy are effective ways to optimize hormonal imbalances to improve spermatogenesis.
- Sperm retrieval is an advanced procedure that harvests sperm within the male reproductive tract so that it can be used to fertilize an egg. Sperm mapping helps Dr. Turek to locate sperm before retrieval for higher success rates.
- Often, simple lifestyle modifications like losing weight, cutting out alcohol, exercising regularly, eating a balanced diet, and reducing stress are sufficient to improve sperm production.
Diagnose Potential Spermatogenesis Problems with a World-Famous Fertility Expert
If you and your partner have had trouble getting pregnant, the first step to becoming a parent is determining the factors that are contributing to infertility. This is called a “root cause” analysis and it is important because it can identify often simple and potentially treatable issues that improve fertility. The Turek Clinic offers diagnostic tests that can pinpoint the likely causes so that a customized treatment plan can be developed. Because of Dr. Turek’s lengthy track record of helping men who were deemed “infertile” by other doctors to become fathers despite spermatogenesis problems, he is one of the country’s top choices for male fertility care. To schedule a consultation, please call 1-888-TUREKMD today.









