Male Infertility Evaluation

For many years, there has been an assumption in reproductive medicine that male infertility due to impaired semen quality is treatable with In Vitro Fertilization (IVF) or IVF-ICSI (In Vitro Fertilization with Intracytoplasmic Sperm Injection). Although many couples conceive using these technologies in cases of male factor infertility, just as many—or more—do not. Hence, the validity of this assumption must be called into question.
Having Trouble Conceiving? We Can Help
Unexplained infertility, recurrent miscarriage, failed IVF, ICSI or IUI? We’ve helped thousands of couples just like you get pregnant!
With the development of more advanced sperm function assays including sperm DNA fragmentation, sperm aneuploidy, measures of oxidative stress and sperm epigenetics, it is now clear that significant male infertility issues may be present in men who:
- Have otherwise normal semen quality,
- Have advanced paternal age (>50 years).
Because sperm testing has improved, it is now possible to ascribe more cases of unexplained infertility (and related losses) to the male partner than ever before.
On the other hand, when couples with unexplained infertility have a formal male factor evaluation in my practice, and I “clear” the male partner without medical or surgical treatment, the natural conception and overall (includes ART) pregnancy rates the year following this evaluation at 65% and 85% respectively (Shin et al, 2015). These pregnancy rates rival anything that reproductive specialists can offer to treat couple infertility.
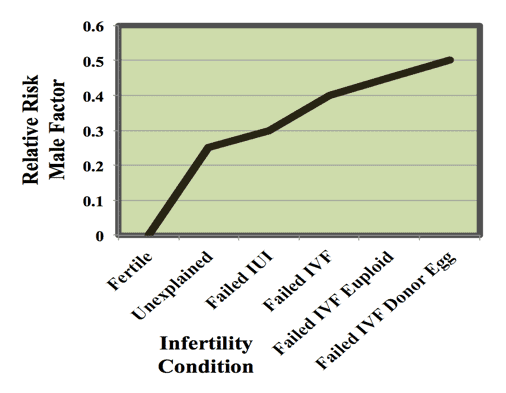
So, when fertility is unexplained or IVF fails, it may very well be due to male factor issues. The precise contribution of male factors to these failures is currently unknown but it has been estimated to reside in 25-50% of cases. The relative risk of male factors by infertility condition is outlined in Figure 1.
Maybe It’s Him®™ Fertility Evaluation

The Maybe It’s Him®™ Evaluation by The Turek Clinic is a straightforward, single-visit, holistic assessment of the relative risk that men bring to bear on a couple’s fertility that goes far beyond what can be evaluated and solved at a typical fertility clinic.
Using the latest tools of the trade, including sperm DNA fragmentation, sperm aneuploidy and epigenetics, this evaluation assesses the male factor risk to natural or ART conception failures. The goal of the evaluation is to calculate the relative contribution of the male factor to the couple’s infertility issue and to provide feedback to that will:
- Change or improve future ART cycle planning, and/or,
- Identify treatable male factor issues that could improve IVF outcomes.
As healthy reproduction requires a healthy body, the full gamut of lifestyle alterations and both classical and alternative medical treatments are employed in treatment recommendations.
Candidate couples for the Maybe It’s Him®™ Evaluation include:
- Unexplained infertility
- Recurrent miscarriage
- Failed IUI
- Failed IVF
- Failed multiple IVFs
- Failed IVF-ICSI
- Failed multiple IVF-ICSI
- Failed IVF-ICSI with euploid (genetically tested normal) embryos (aka failed embryo transfer)
- Failed IVF-ICSI with donor egg
So, if your IVF cycle failed, or are looking for answers why that euploid single embryo transfer did not take when it should have, then consider a Maybe It’s Him®™ Evaluation at The Turek Clinic now.
Potential Treatment Options
Based on the results of the Maybe It’s Him®™ Evaluation, Dr. Turek can tell you where you stand and recommend potential treatment options to improve the likelihood of you and your partner conceiving.
Every patient is unique, and Dr. Turek’s treatment recommendations will be individually tailored to the specific factors that are causing or contributing to your fertility problems.
Medications for Hormone Support
You will have bloodwork to check how well your body is producing certain fertility hormones. If the results show abnormal levels of testosterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol and/or prolactin, Dr. Turek may suggest balancing out your hormones with medications. Clomid and Anastrozole have been shown to offer hormone support and in some cases, increase sperm count. HCG and FSH injections are more potent alternatives to clomid that are also used in selected cases.
Lifestyle Changes
Making lifestyle modifications may help improve your chances of conceiving a child. Dr. Turek will discuss your lifestyle with you, inquiring about any behaviors, such as smoking marijuana, using other recreational drugs or frequently enjoying hot tubs, which can impair sperm count and sperm quality. He will also go over your medications to look for any prescription or over-the-counter drugs that could interfere with your fertility. It’s also very true that your body weight matters to fertility, and recommendations regarding weight management might be made.
Making smarter lifestyle changes or altering medications may improve your ability to conceive. Adding a natural or holistic supplement such as AlphaSperm or consuming more antioxidants in your diet can also make a difference.
Diagnostic Treatments
Sometimes Dr. Turek needs more information before recommending a course of treatment.
For example, by performing an ultrasound, Dr. Turek can look for abnormalities or blockages in your reproductive tract that block the sperm path. If he finds something, he may recommend surgery to correct it.
Sperm mapping™ can tell Dr. Turek whether your testes are producing sperm and if so, the amount and location of the sperm. Using the fine needle aspiration technique, Dr. Turek takes small samples from your testicles and examines them under a microscope to look for sperm. He then organizes the findings into a map that can be used for sperm retrieval. Sperm mapping™ is minimally invasive, does not require incisions and does not cause stress or much pain for patients.
Surgical Solutions
A varicocele, or enlargement of the veins in the scrotum, is a common problem that can hinder sperm production. Approximately one-third of the men that Dr. Turek evaluates for infertility have varicoceles. In many cases, repairing a varicocele with surgery can improve a man’s chances of fathering a biological child. Dr. Turek helped to popularize the microscopic subinguinal microsurgical approach to varicocele repair; it is the most successful approach and the least likely to cause complications. He will usually want to rule out other male infertility causes, such as an obstruction of the reproductive tract, before recommending surgical varicocele repair.
Blockages in the reproductive tract can lead to either low numbers of ejaculated sperm or no ejaculated sperm. In many cases these are correctable with surgery. In some cases, the blockage is near the prostate (ejaculatory duct obstruction) and is treatable with endoscopic surgery. In other cases, it may require microsurgical repair within the scrotum. Dr. Turek has published his techniques and success rates for treating such conditions.
Should sperm mapping™ reveal usable sperm in the reproductive tract, Dr. Turek may suggest sperm retrieval. The retrieved sperm are then used for assisted reproduction (e.g., in vitro fertilization and intracytoplasmic sperm injection). There are several safe, effective and minimally invasive sperm retrieval techniques; Dr. Turek will go over your options and help you decide on the most appropriate choice.
Frequently Asked Questions About Getting a Male Infertility Evaluation
How invasive is a male infertility evaluation?
A male infertility evaluation is not invasive or painful at all. Expect to receive a thorough physical examination and an in-depth discussion of your medical history. Lab-based testing may be performed, too. You will need to give or have had at least two semen samples. Depending on the results of these tests, additional testing, such as ultrasounds or more thorough testing of semen quality, may be recommended.
How can I best prepare for my evaluation?
Refrain from ejaculating for two to three days before your visit in case Dr. Turek orders your semen analysis testing the same day as your appointment.
Also bring your past medical records, including information about any prior infertility assessments or treatments performed on either you or your partner. It is helpful to compile a list of medications you currently take.
Be prepared to answer questions about your lifestyle, medical history, any current stressors or symptoms you are experiencing and habits regarding smoking, alcohol and other drug use.
Finally, feel free to bring a list of any questions you have for Dr. Turek so you don’t forget them during the appointment.
At what point should I consider undergoing a male infertility evaluation?
A male infertility evaluation is generally recommended if you have not conceived after one year of having unprotected, regular intercourse. However, if your partner is 35 or older, or if you have a history of reproductive health issues, you may want to seek Dr. Turek’s advice after six months of trying to conceive.
What is sperm DNA fragmentation?
Sperm DNA fragmentation testing evaluates the integrity of the genetic payload in sperm. It does not assess the sperm chromosomes or mutations in DNA. It simply looks at the packaging quality of the sperm DNA, which correlates to a man’s natural fertility and also to the failure of assisted reproduction. It is another tool Dr. Turek can use to assess your fertility potential.
Since abnormalities in sperm DNA fragmentation are correlated with lifestyle choices, paternal age and overall health, this testing can provide us with key clues about causes of infertility and help guide fertility treatment.
How can sperm DNA fragmentation be treated?
Decreasing oxidative stress may decrease the amount of damage to sperm DNA. Common recommendations include eating a diet rich in antioxidants and making healthy lifestyle choices, such as not smoking, exercising regularly and limiting alcohol consumption.
What does “sperm aneuploidy” mean?
A sperm aneuploidy test evaluates the presence of abnormalities in the number of chromosomes in sperm. The results of this assessment can shed light on the ability of sperm to create healthy embryos and explain cases of miscarriages.
What is epigenetics and how does it affect male fertility?
Epigenetics is any process that alters gene activity without changing the DNA sequence. It is not a measure of chromosomal integrity or mutations in DNA. Research suggests that sperm epigenetic patterns can predict your ability to father children, both naturally and with the help of assisted reproductive technology.
Are at-home sperm testing kits a substitute for a professional evaluation?
No, at-home sperm tests cannot replace a professional evaluation and laboratory-based sperm tests. In-office assessment and laboratory testing provide a much more complete picture of fertility and potential barriers to fertility. At-home sperm testing is less rigorous and complete than laboratory-based testing, often measuring only two or three of 13 features examined by lab-based testing.
References
- Shin D, Christensen EC and Turek PJ. A prospective study of natural pregnancy rates in “cleared” male factor couples. J. Urol. 2015, 193: Suppl e946.
- Blázqueza A, García D, Rodríguez A, Vassena R, Vernaeve V. Use of donor sperm in addition to oocyte donation after repeated implantation failure in normozoospermic patients does not improve live birth rates. Hum Reprod. 2016, 31:2549-2553.
- Bhattacharya S, Maheshwari A, Mollison J, Factors associated with failed treatment: an analysis of 121,744 women embarking on their first IVF cycles. PLoS One. 2013 Dec 5;8(12):e82249.
- Walschaerts M, Bujan L, Parinaud J, Mieusset R, Thonneau P. Treatment discontinuation in couples consulting for male infertility after failing to conceive. Fertil Steril. 2013, 99(5):1319-23.
- Tournaye H. Male Factor Infertility and Art. Asian J Androl. 2012, 14:103-8. (Review)
- Garrido N, Bellver J, Remohí J, Simón C, Pellicer A. Cumulative live-birth rates per total number of embryos needed to reach newborn in consecutive in vitro fertilization (IVF) cycles: a new approach to measuring the likelihood of IVF success. Fertil Steril. 2011, 96:40-6.
- Dodge L et al. Age of Men Affects IVF Success. ESHRE talk July 2017.
- Liu Z, Shi X, Wang L, Yang Y, Fu Q, Tao M. Associations between male reproductive characteristics and the outcome of assisted reproductive technology (ART). Biosci Rep. 2017 Jun 27;37(3) (636 couples, single IVF center).
- Oleszczuk K, Giwercman A, Bungum M. Sperm chromatin structure assay in prediction of in vitro fertilization outcome. Andrology. 2016; 4:290-6
- Bungum M, Bungum L, Lynch KF, Wedlund L, Humaidan P, Giwercman A. Spermatozoa DNA damage measured by sperm chromatin structure assay (SCSA) and birth characteristics in children conceived by IVF and ICSI.









